 Solved: Which Of The Following Statements Is True Regardin... | Chegg.com
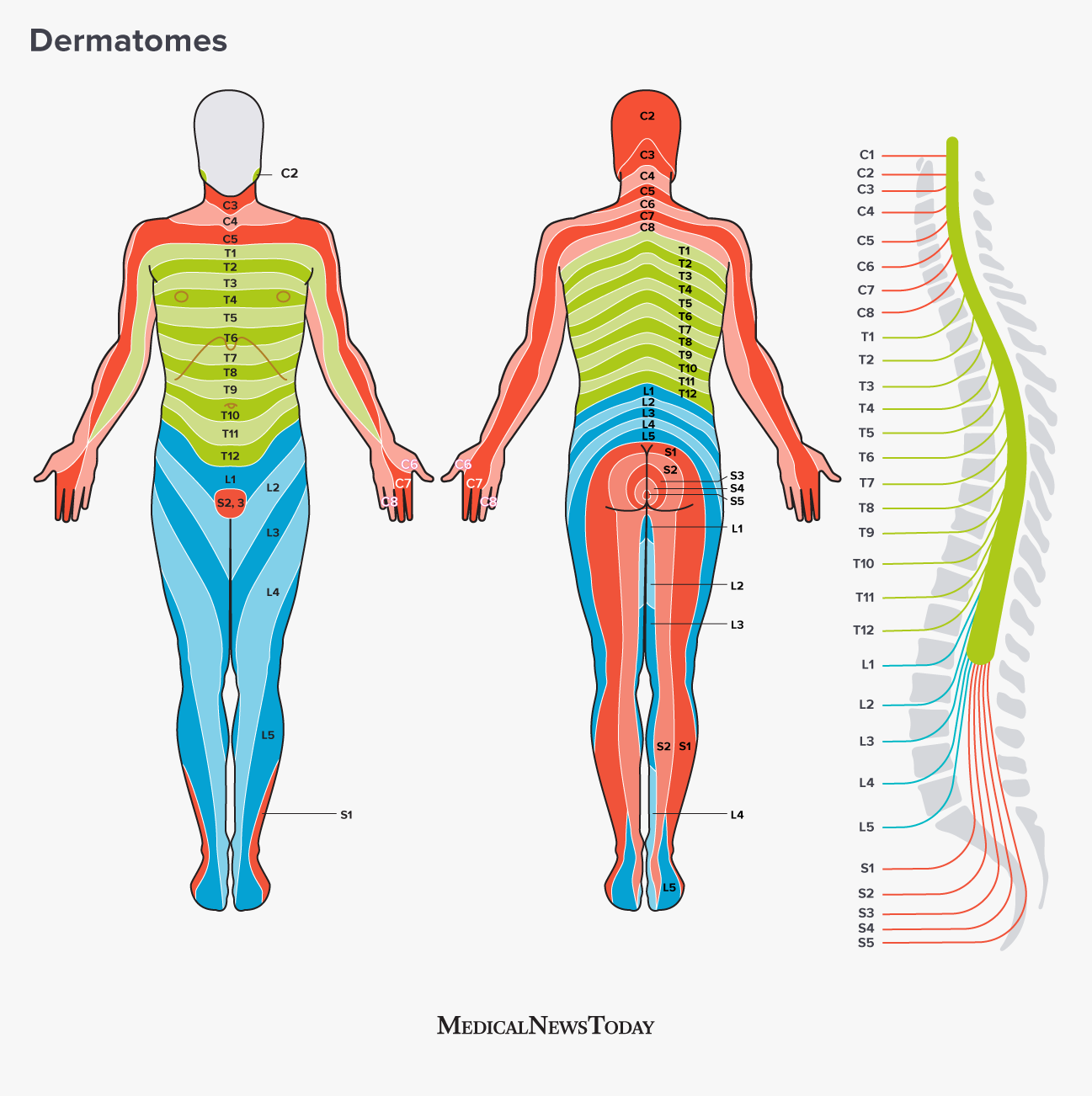
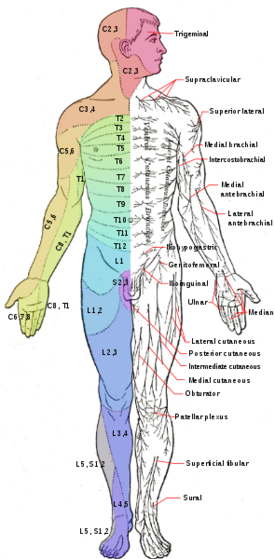
Solved: Which Of The Following Statements Is True Regardin... | Chegg.comDermatomeDermatoms are mainly used to determine whether the sensory loss in a limb corresponds to a single spinal segment, which implies that the lesion affects that particular nerve root (i.e., radiculopathy) and assign a neurological "level" to a spinal cord injury. From: Related Terms: David L. Felten MD, PhD, ... Mary Summo Maida PhD, in , 20169.19 Distribution Dermatomal A dermatoma is the skin area supplied by a single spinal nerve root; the cellular bodies are found in dorsal root nodes. Spinal nerve roots are distributed in structures according to their associations with segments of the spinal cord. The nerve roots that supply neighboring dermatomies overlap. Thus, the section or dysfunction of a single dorsal root produces hypoesthesia (reduced sensation), not anesthesia (total loss of sensation) in the region supplied predominantly by that dermatoma, as shown in the figure. Dermatoma anesthesia requires damage to at least three dorsal roots: the central dorsal root and the roots above and below. Instead, an irritative lesion such as an herniated intervertebral disk can cause acute and radiant pain within the distribution of the affected dermatoma. As the lower extremity buds develop, they remove the nerve roots that correspond to their mesoderal cores and ectodermal covers. The lower extremities in development revolve around a longitudinal axis, with an oblique orientation resulting from the dermatoms. L1 and L2 dermatoms can be found on sites adjacent to S2 and S3 dermatoms due to the intervention segments that migrate in more distal parts of the lower extremities. Knowledge of dermates is important for the location of lesions of the peripheral nerve root and distinguish them from peripheral nerve lesions. In, 2007DERMATOMESI. DEFINITION Dermatomas define the area of the skin interiorized by a single nerve root or spinal segment. They are mainly used to determine whether the sensory loss in a limb corresponds to a single spinal segment, which implies that the lesion is from that nerve root (i.e., radiculopathy) and assign the neurological "level" to a spinal cord injury. II. DERIVATION OF THE DERMATOMAL MAPS The original human maps arose from Sherrington experiments with monkeys and Head observations of patients with herpes zoster infection.2,38 These maps have been revised later, based on several types of tests collected during the last century, including neurosurgical observations (by Cushing, Foester and Keegan), experiments that inject novocaine along with the nerve roots of the students. 1,2,38–40 Differences between dermatomas maps, which are minor and relate mainly to the proximal extension of some dermates of members, probably reflect biological variations and differences in the experimental method (i.e., the sensory loss of a hernia disc or novocana injection is not necessarily the same as that of root resection). III. TECHNIQUE The map dermatomal in the Fig. 58-1 is the international standard used to classify patients with spinal cord injury (Table 58-1).41 Two principles apply when evaluating the dermatoma pattern of sensory loss: (1) Contiguous dermatomes overlap, which means that damage to a nerve root can cause anesthesia or a sensory loss confined to a small area. These small areas, which are called "signature zones", define the sensory level in patients with spinal cord disease. * (2) Touch dermatomy is bigger than pain dermatomy. This suggests that when only one or two segments are affected, the pain sensitivity test is a more sensitive test method than the abnormal touch test.1.2IV. CLINICA SIGNIFICATION The sensory level of the patient is often several segments below the actual level of the spinal injury (e.g., the patient with a T8 sensory level may have a T3 segment injury in the spinal cord). *42–45 There are two explanations for this phenomenon: one is that the organization of the ascending pathway (with pain and feeling of temperature) makes the lateral fibers that carry lower sensations of the body more vulnerable to external injury. Another is that the actual spinal injury causes injury by compromising the blood supply of the rope, causing injury to a distant segment.42.43 When sensory levels and engines are not in agreement, the level of the engine is a more reliable indicator of the level of injury and future disability for the patient. 47 In some patients with spinal cord disease, the most accurate indicator of the affected spinal segment is the site of the patient's pain and vertebral tenderness or the level of the patient's root pain. 44,48The clinical meaning of the dermatoma sensory loss in disorders of nerve roots is discussed in Chapter 60. Jane E Carreiro DO, in , 2009LOCATIONDermatoms, myotoms and sclerotomies are sensory inervation areas associated with a common nervous root. These areas were first described at the end of the century by the Head and are called the "head areas". A Cabeza area represents the sumotion of dermatoma, miotome and sclerotronomic patterns that have the same embryonic origin, i.e., invation pattern. Each of these types of tissues has different densities of receptor cell types. The skin receptors generally respond to a light touch, two-point discrimination, temperature and nociception. Muscle receptors are activated by nociception, stretching and chemical signals. Bone and periosteum receptors respond to nociception and tend to have higher thresholds for activation than those of other tissues. A signal from a spinal cord level like T1 will be interpreted by the somatosensorial cortex as coming from one of the areas of the Head. For example, irritation of the nerve root can present as pain that radiates the limb in a dermatoma distribution. However, if the pain generator is the disk, the pain can be expressed as boring and boring in the distribution of sclerotomus. Nociceptive stimulation of the tissue in any particular area will activate the cells in the backbone of that spinal cord area. In many situations, the same neuronal cells can receive information from three different types of tissue: skin, bone, and muscle. This information will be transmitted to the brain. The cells of the cortex learn to interpret the signals of the spinal cord as from specific tissues, based on the intensity and frequency of the signal and the location of the activated cell. For example, a signal that travels along the anterolateral system (ALS) from the T4 area of the spinal cord may have originated in the shoulder or heart. The T4 signal is transported by many neurons, some of which will be mapped to specific cells in the somatosensorial cortex, and others less specific. Cortical cells can recognize the location of the signal source by the company it maintains. The cells also "learned" to associate the activity at a certain level of the spinal cord with irritation to a specific tissue. However, if the inciting spinal cord cell or the receptor cortical cell receives input from more than one type of tissue, the cortex may not be able to differentiate between them. This is one of the mechanisms of the pain referred to. An irritation or injury to a body area is interpreted as coming from a different tissue because both have a common inervation. Shared inervation is more common between a visceral organ and a somatic tissue than between two somatic tissues. Clinically, we often associate this process with visceral pathology. Most of the spinal cord sensory cells that receive somatic tissue input will also receive viscera input. When the brain receives a signal from that area of the spinal cord, it cannot distinguish between visceral and somatic tissue. If, during life, the cortex has learned to interpret pain stimulation from the T4 area as an injury to the arm or shoulder, then when T4 becomes stimulated by myocardial injury, the brain can continue to interpret that signal as shoulder pain. Many related pain incidents, such as shoulder irritation with gallbladder disease, and back pain with urinary tract infections, can be explained by the convergence patterns of the Cabeza areas. For most people, the brain is initially exposed to signs of somatic tissue pain rather than visceral. The brain learns to interpret nociceptive signals from most areas of the spinal cord as from somatic tissue. Thus, the symptoms of visceral pathology refer to the musculoskeletal system. However, when children develop early visceral diseases such as reflux, intussception or surgical correction of congenital heart disease, the brain learns to interpret the nociceptive entry of those areas of the spinal cord as visceral irritation rather than somatic. Later, when somatic irritation develops, the child may complain of symptoms similar to those associated with early visceral pathology. S. Jacob MBBS MS (Anatomy), in , 2008Recognition of dermatoms (spiritual skin invasion) and myotoms (egemental muscle intravation) are important for the nerve root compression test and the evaluation of the spinal cord injury level (Fig. 2.38). The dermats of the upper segments of the brachial plexus (C5, C6) are on the side side side, the lower segments (C8, T1) in the middle side and C7 in the center. There is a considerable overlap between adjacent dermatoms. However there is no overlap through the axial line as it separates discontinuous segments. Swetal Patel, in , 2015Head and Neck The map dermatoma starts with the trigeminal nerve and its distribution on the head and neck. The trigeminal nerve is divided into three branches: the ophthalmic branches (V1), maxilla (V2) and mandibular (V3). The ophthalmic branch is responsible for carrying sensory information from the tip of the nose to the scalp and the forehead. The maxillary branch covers the area from the upper lip and the buccae. The mandibular nerve covers the area from the lower lip to the lower part of the jaw and parts of the outer ear (Gray, 2006). C2-C4 cover the skin below the angle of the back mandible part of the ear and the side and previous parts of the neck. C2-C6 cover the back of the neck where C2 is responsible for the upper aspect and C6 the lower part (Gray, 2006; Figure 34.1). Figure 34.1. Map of the head and neck dermatoma showing the trigeminal distribution along with the C1-C6 cervical distribution. Stephen M. Russell MD, John E. McGillicuddy MD, in , 2012 Sensitivity tests in patients with brachyal plex lesions Dermatoma C5 covers the side of the shoulder and arm to the elbow (Figure 3.15). The sensitivity of this area is carried in part by the upper side rib of the axillary nerve, as well as the lower side nerve of the proximal radial nerve. The lateral forearm and thumb are the sensory territory of the C6 spinal nerve. This sensation is carried in part by the lateral forearm skin nerve of the muscutaneous nerve, and for the thumb, by the terminal sensory branches of the medium nerves (surface fly) and radial (surface smell). An injury involving the upper trunk, or alternatively the C5 and C6 spinal nerves, causes a sensory loss that involves the lateral half of the arm and the forearm, as well as the whole thumb. The flying and dorsal aspects of the long finger are almost exclusively within the C7 dermatoma. The sensory division of the medium nerve (smooth of the finger and nail bed) and the surface sensory radial nerve (sense-sided aspect) carry this feeling. The lesions of the middle trunk, composed only of C7 fibers, logically cause the same pattern of sensory loss as does a pure C7 palestra. The C8 dermatoma covers the medium, or ulnars, one third of the hand, including the small finger and the lateral hypotenar eminence. The skin nerves and palms of the ulnar dorsal ulnar, together with the superficial sensory division of the ulnar nerve, bring sensation from this area. The T1 sensory dermatoma covers mainly the medial half of the forearm, with its sensory fibers being transported by the mid-arbrachial skin nerve, a distal branch of the median cord. A lower trunk, or the combination of C8 and T1 nerve lesions, causes a sensory loss in the medial part of the forearm and hand, including the small finger. It should be noted that the medial arm is mainly covered by the T2 dermatoma, with the arm (and some proximal medial arm) covered by T3. Lynne Gaskell, in , 2013 Neurological TestsThe compression or traction of spinal nerve roots by transgression of disk and/or osteophytes can result in related pains, paraesthesia and anesthesia, and also give positive neurological signs. Neurological signs should be carefully monitored as deterioration can indicate worsening pathology. Dermatomas A dermatoma is a skin area supplied by a particular spinal nerve. The dermatomas can exhibit sensory changes for light touch and pin prick. Try each dermatoma individually, on the unaffected and then on the affected side. Myotomies A myotomo is a muscle supplied by a particular nervous root level. These are evaluated by performing resisted isometric tests of the L1–S1 myotoms in medium range, sustained for approximately three seconds. Try the unaffected side, then the affected one: LI–L2 for the hip flexors (see Figure 11.13), L3–L4 for the knee cumuls (see Figure 11.14), L4 for the foot flexors and invertors, L5 for the extension of the large finger, S1 for the plant bending (see Figure 11.15) and the knee pelicula, S2 for the affected foot bending Note: boring reflections can indicate minor neuron dysfunction. Risk reflexes may indicate a dysfunction of superior motor neuron. L3 corresponds to the quadriceps. The patient sits with the flexed knee and the therapist strikes the patellar tendon just below the patella (Figure 11.16). S1 corresponds to the planters. Dorsiflex the ankle and hit the Achilles tendon. Observe and feel the bending plant in the ankle (Figure 11.17). Clinical Note The Babinski reflex (or plant response) is an abnormal response and occurs when a blunt object draws the side aspect of the foot plant. Normally, the big toe-ups (great toe). Normally, the big finger extends by indicating damage of superior neuron engine. Note that this primitive reflex is seen in the newborn but disappears over time. Adverse mechanical tension The patient is supine. The physiotherapist passively reflects the patient's neck. Note any low back pain response, which may suggest disco pathology. This is also known as the Lasegue test. The patient is supine. The physiotherapist lifts the patient's leg by maintaining the extension of the knee (Figure 11.18). An abnormal finding is back pain or sciatic pain. The ciatic nerve is in full stretch at approximately 70 degrees of bending, so a positive sign of the cyatic nervous involvement occurs before this point (Palmer and Epler 1998). Any response to pain and range of movement is observed and compared to the other side. Factors such as hip aduction and medial rotation further sensitize the ciatic nerve; the ankle dorsiflexion will sensitize the warm portion of the cyatic nerve; plant bending and investment will sensitize the peroneal portion of the nerve. The patient is prone and the physiotherapist flexes the person's knee and then spreads the hip (Figure 11.19). Pain in the back or distribution of the femoral nerve indicates irritation of the femoral nerve or reduced mobility. The comparison is made with the other side. This testifies to the mobility of the hard mater. The patient sits with the thighs fully supported with the corrected hands behind the back. The patient is instructed to deplore the shoulders to the groin (Figure 11.20). The physiotherapist applies a gentle overpressure to this bending of the trunk. The patient adds cervical bending, which is maintained by the therapist. The patient then performs the unilateral active knee extension and the active ankle dorsiflexion. The physical therapist should not force the movement. The unaffected party should be evaluated first. Any symptom is observed in the particular part of the range. If the hard mat is tethered, the symptoms will increase as each component is added to the decline test. The patient has instructions to extend the head – a reduction in symptoms in the cervical extension is a positive finding, indicating abnormal neurodynamics. Lumbopelvic stability tests The stability of the lumbar column is necessary to protect the lumbopelvic region from the daily demands of posture and load changes (Panjabi 1992). It is essential for normal painless activity (Jull et al. 1993) and should always be evaluated. With the coconut patient lying with the hips at 45 degrees of bending, he is instructed to maintain a neutral column (it may be useful to tell the patient to keep such a syrosis that an army of ants could crawl through!). The person then performs an abdominal en-drawing by contracting the transverse abdomini muscle while trying to keep the spine neutral. To challenge transversus abdominis and multifidu stabilizing muscles (and therefore the spinal position), the patient adds the leg load by alternatively lifting the ground heels and sliding the leg by maintaining a neutral column position. The maintenance of a neutral column posture can be evaluated using a biofeedback device. An inability to keep the spine in neutral will result in the lumbar spine extending as the leg rises. The intraabdominal pressure mechanism is controlled mainly by the diaphragm and transversus abdomini that provides a hardening effect on the lumbar spine (Hodges and Richardson 1997). PalpationThe spraining of soft tissues on the joint pillar in one or more levels of spina dorsal is a common finding in cases of degenerative disease of the lumbar spine, such as the thickening and prominence of the hard booty on the apophiseal joints. Note any general stiffness or localized thickening of muscle tissue or ligament tissue. In general, the greater the change of soft tissue, the harder they are; the more recent, the softer they are. However, a thick or stiff area is not necessarily painful or the source of a patient's symptoms (Maitland 2001). Spinal movements accessories The physiotherapist applies central posteroanterior pressures on the splendid processes and unilateral pressure (one face) on the joint pillar (Figure 11.21), pointing out areas of hyper and hypomovility. Record any pain experienced by the patient and the corresponding column level. Case study A 30-year-old worker was referred to for physiotherapy following an occupational elevation injury. He complained of the lower back on the left side and pain of the medial tincture, and intermittent paraesthesia that affected his left finger. The pain was aggravated by bending and relieved by foot and walking. When I examined, I had a marked change to the right. Flexibility was reduced to the tip of the fingers to the knees and its left SLR was reduced to 50 degrees. Due to the rapid appearance of symptoms associated with a lifting injury in a flexive posture, and the pain aggravated by bending and relieved by extension activities, the injury was hypothesized to be discogenous. Clinical trials suggest that the most common sources of low back pain are intervertebral disk, zygapophyseal joint (photo) and sacroiliac joint (Maitland 2001). The patient was treated by rotations to the right (as was shown in another patient in Figure 11.22), which centralized his pain. His turn was manually corrected on the first visit. Repeated prone extension exercises were prescribed, as McKenzie (1985) advocated, to do at home every two hours. On the third visit his pain had been centralized to leave the back pain low and his SLR had 80 degrees. Then it was treated by unilateral mobilizations to the left to grade 4. This relieved your symptoms and recovered the entire range of movements. Before the discharge, a program of abdominal and multifidu exercises was given. They also gave her posture and ergonomic advice before her return to work. Multifidus and abdominus cross-sectional muscles have been considered primarily responsible for providing local stability to the lumbar column in the neutral zone of the joint (Panjabi 1992; Goel et al. 1993; Wilke et al. 1995; Hodges and Richardson 1996). Robert Gaiser, in , 2011 Surgical Stages Variety of dermats available to cut STSG. In general, the dermatomies driven by air or electric and the open-hand knife are used to cut longitudinally into the extremity; drum dermatomy used on the back through the extremity. Width of graft determined by the width adjustment in dermatome If betadine is used to prepare the donor area, it should be washed to avoid the sticker. Deep lubricated skiing with sterile mineral oil to facilitate grafting Advancing flat dermatoma through the skin with soft downward pressure Cleaned with saline or betadine solution Surgical debridation can cause bleeding; significant hemostasis for the survival of the grafted Hilo placed in the wound, sutured around the periphery, and dress. The main purpose of the dressing is to ensure the contact between the graft and the host bed. Dress to the left instead for ¦7 d, at the time you can remove the sutures. Reasons for graft failure: inappropriate bed (poor vascularity), hematoma, movement, infection, technical errorsEBL: Depends on the extension of the graft, minimum to 250–500 mConsideration of the activityAnotation of the pain: 4–6Application of the lidocaine sprayer to the donor site reduces postoperative pain Minimum level for the first 2 d after surgeryMonito Heat los ORM M. Danzl PT, DPT, PhD, NCS, M.R. Wiegand PT, PhD, in , 20172 What are common dermatoms tested in a higher and lower trimester screening test? Side-footed outermost partSleeping-thin-thin-thin-thin-thin-thin-the-thin-thin-the-sided-thin-thin-the-sided,thin-the-sided,thin-the-sided,thin-the-sidedum-thin-thin-thin-thin-thin-thin-thin-thin-thin-thin-thin-thin-thin-thin-thin-thin-thin-thin-thin-thin-thin-thin-thin-thin-thin-thin-thin-thin-thin-thin-thin-thin-thin-thin-thin-thin-thin-thin-thin-thin-thin-thin-thin-thin-thin-thin-thin-thin-thin-thin-thin-thin-thin-thin-thin-thin-th They have more capillaries exposed in their subsurface compared to total disease grafts, which allows greater absorption of nutrients from the wound bed. In addition, the skin grafts of digestion consist of less tissue that requires revascularization. As a result, divergence grafts are often used for wounds in which revascularization is a matter of concern. However, due to its probable bad color and texture match normal skin and its tendency to contract, divergent skin grafts are used selectively in facial reconstruction. Some indications of dyspnea skin grafts include covering too large defects to repair with a local flap (Fig. 15-20), to facilitate the monitoring of the possible recurrence of cancer, and provide temporary coverage of a wound bed prior to final reconstruction (Fig. 15-21). Most division thickness grafts are between 0.012 and 0.030 inches thick, with thicker grafts that have a relatively better color and texture match the facial skin. 3Technique Electrical The brown dermatoma is a device commonly used to harvest dyspnea skin grafts, usually of the anterolateral thigh (Fig. 15-22). The dermatoma is mounted before use, placing the disposable metal sheet on the project rivets. The screws at the back of the dermatoma are tight and the device is calibrated. The calibration involves fixing the dermatoma dials to zero and then moving both dials simultaneously to set the graft thickness dial to 15 thousandths of an inch, which corresponds to the passage of the hinge portion of a Bard-Parker No. 15 blade between the blade and the cap. The donor site is marked, with the length of the graft equal to the larger dimension of the host site, plus an additional 15 to 20% in anticipation of any grafting contraction.3 Grafts can be harvested under general anesthesia without using a local anesthesia. If the patient receives intravenous sedation or not sedation, a local anesthesia consisting of 1% of lidocaine with 1,100 000 concentration of epinefrine is subcutaneously injected. After skin preparation, mineral oil is placed on the donor site. While the surgeon provides contraction with his nondominant hand, an assistant provides traction with a tongue blade on the top look of the donor area. The pressure of light down is applied by the dermatoma at the donor site while the dermatoma is advanced. The forceps are used to prevent the graft from being trapped in the dermatoma, and at the end of the donor area the dermatoma rises away from the skin while it is still cut. This facilitates the adhesive tape of the graft in that area. Divergent skin grafts are reinforced in the wound bed in a manner similar to all types of skin grafts. Before placing a compression deposit, small incisions can be made in the graft at even spacing intervals to allow liquid discharge during the healing phase. The care of the wound after the removal of the seam is the same as that of the grafts of the complete disease. A sterilized gas dermatoma commonly used in the O.R. is the Padgett dermatoma (Fig. 15-23). This dermatoma comes with three templates, allowing grafts with widths of 2, 4 or 6 inches to be harvested. It is not necessary to calibrate, and the grafts are harvested in a similar way as with the Brown dermatoma. The wound of the donor site is dressed with soaked gauze in hydrogen peroxide to facilitate hemostasis. The gauze is removed, the wound is paddled and a Tegaderm/OpSite sterile dressing is placed. The dry gauze secured by tape is placed on the OpSite as a light compression dressing, taking care not to wrap the tape circumferentially around the leg. Any liquid collection under the tank can be drained after gas removal at 48 h. This is achieved by inserting a sterile needle through the OpSite to vacuum the fluid, then "patching" the needle hole with a small piece of OpSite. The OpSite is left in place for 5 to 7 days, and after the removal the wound is taken care of by daily cleaning with saline and the application of bacitracin and a non-herited gauze dressing. Alternatively, hydrophilic polyurethane (Allevyn), which is highly absorbable and non-adherent, can be used as a donor site dressing.3 This dressing has an external layer similar to OpSite and an internal layer that has an absorbing nature that helps prevent fluid accumulation and leakage. Brodovsky et al suggest that aerosol Nobecutane is an effective temporary dressing for skin graft donor sites.9 The sprayer contains an acrylic resin modified in an organic solvent and disulfido tetrametiuram, which is a bactericidal-fungicidal agent. When sprayed into a wound, the spray forms a transparent plastic film, which is spontaneously shed with epidermal regeneration. 9 Recommended Publications: We use cookies to help provide and improve our personalized service and content and ads. By continuing to accept . Copyright © 2021 Elsevier B.V. or its licensors or collaborators. Direct Science ® is a registered trademark of Elsevier B.V.ScienceDirect ® is a registered trademark of Elsevier B.V.
People also ask William Ch. 13 Vocabulary Silencio Quizlet10.4B: Axon Bundles - Free MedicineTextsNerve - Wikipedia The peripheral nervous system – Anatomy and Physiology Overview of the structure and function of neurons (article) strain Khan Academy The peripheral nervous system - SEER TrainingDuke Histology - Nerve TissueSSB HISTOLOGY Nervous Tissue SAQ - ← SIU School of Medicinethe nervio system - Star Mountain Community CollegeRelated searches
Solved: 45) Which Of The Following Is True Of A Dermatome?... | Chegg.com
AHCDW9Notes28.pdf - 28 Award 10.00 points Problems Adjust credit for all students Which of the following statements is true regarding dermatomes Each | Course Hero
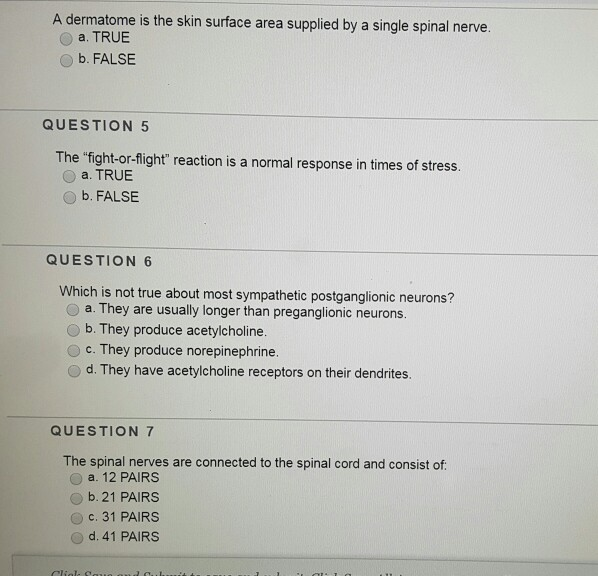
Solved: A Dermatome Is The Skin Surface Area Supplied By A... | Chegg.com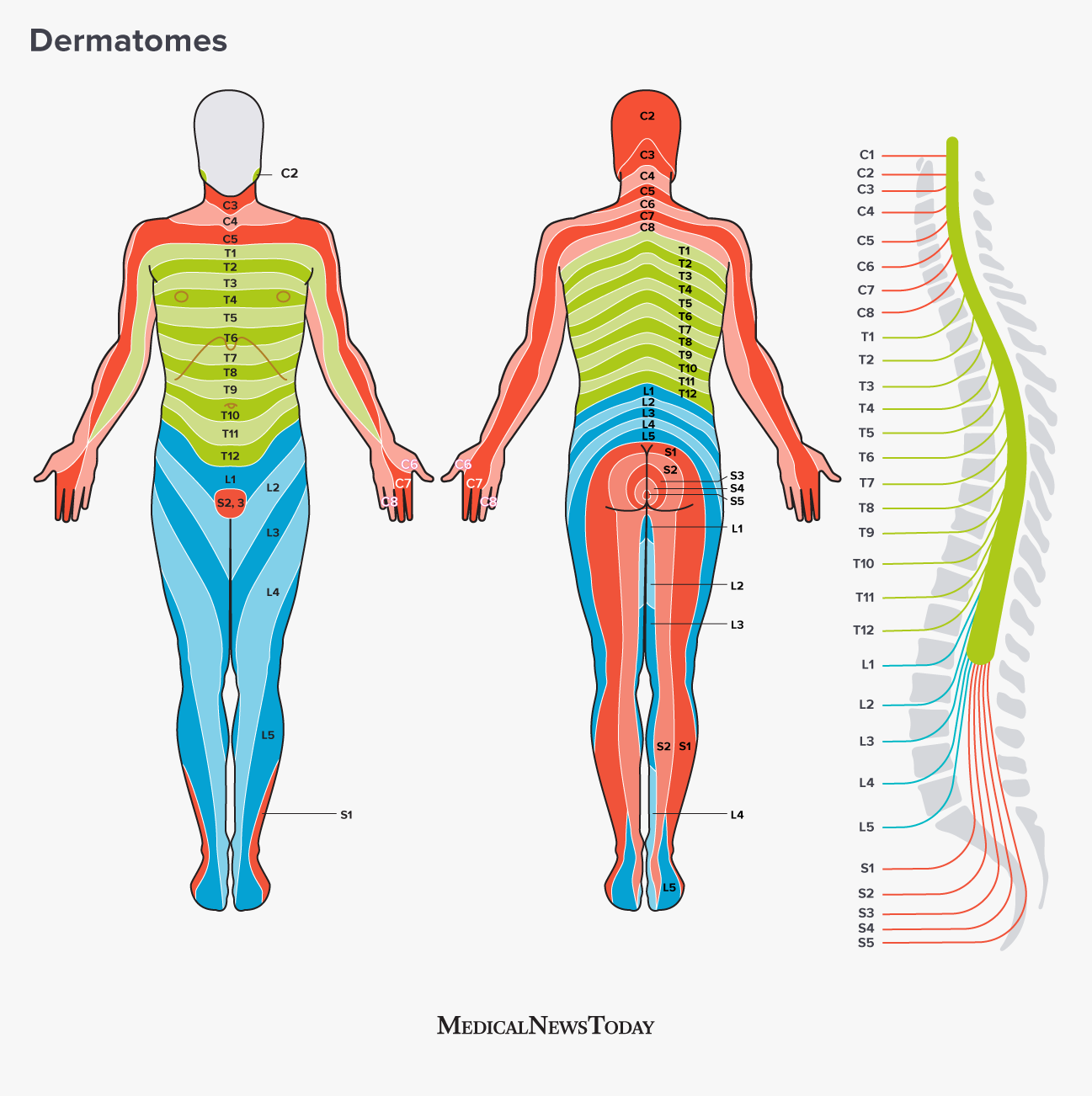
Dermatomes: Definition, chart, and diagram
WEEK 1 QUIZ Diagram | Quizlet
chapter 13 homework Flashcards | Quizlet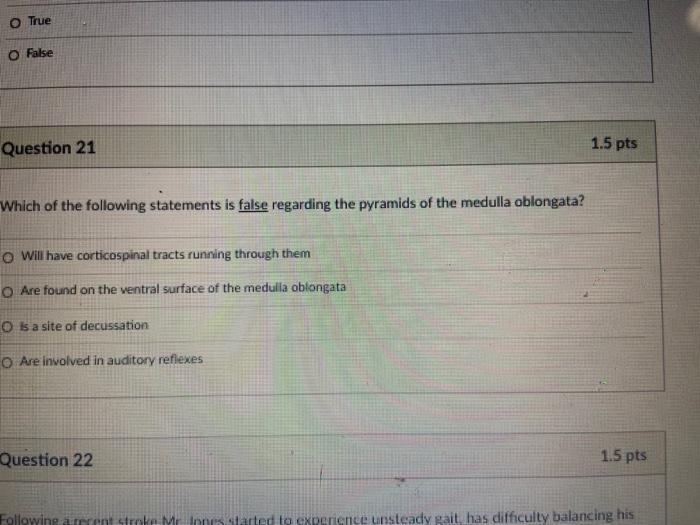
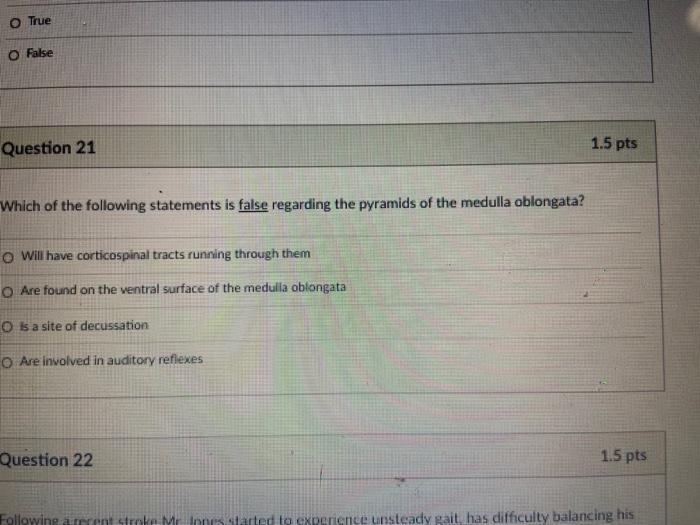
Solved: от OU Og Question 20 1.5 Pts Dermatomes Are Specif... | Chegg.com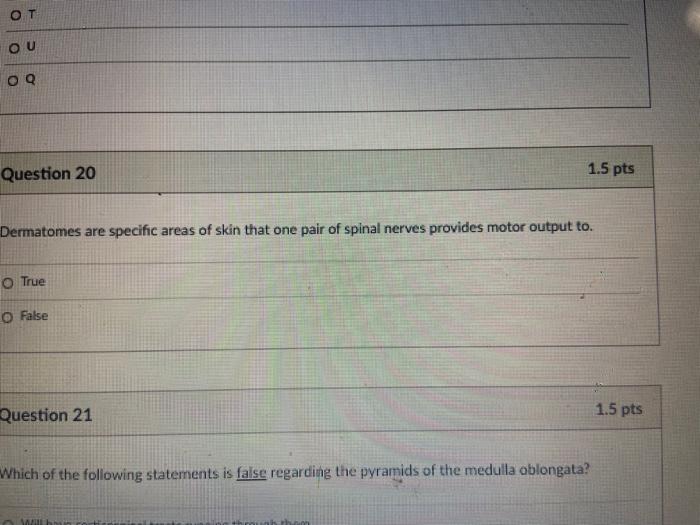
Solved: от OU Og Question 20 1.5 Pts Dermatomes Are Specif... | Chegg.com
Conflicting Dermatome Maps: Educational and Clinical Implications
Clinical Anatomy of the Dermatomes and Innervation of the Joints | SpringerLink
Conflicting Dermatome Maps: Educational and Clinical Implications
Solved Which Of The Following Statements Is True Regardin - Dokter Andalan
Which of the following best describes a dermatome? a) Motor information carried by cranial nerve b) Part of the body innervated by the motor portion of spinal nerve c) Part of the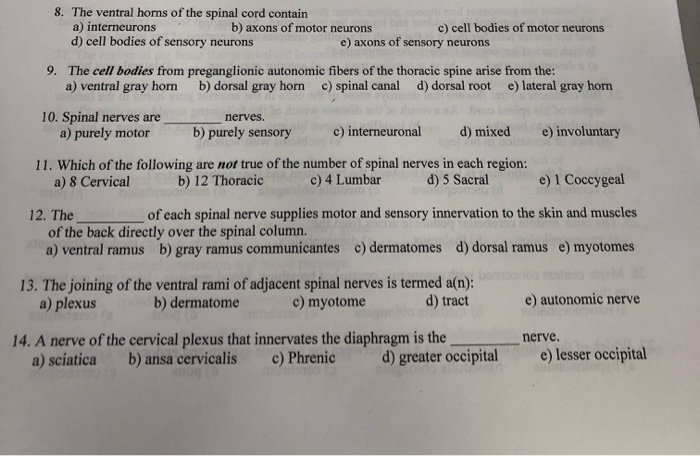
Solved: Answer All Questions. Only Give Correct Answer Cho... | Chegg.com
Clinical Anatomy of the Dermatomes and Innervation of the Joints | SpringerLink
Dermatomes: Definition, chart, and diagram
Spinal Anesthesia - NYSORA
Dermatome (anatomy) - Wikipedia
chapter 13 homework Flashcards | Quizlet
Clinical Anatomy of the Dermatomes and Innervation of the Joints | SpringerLink
Love-hate... and dermatomes
Dermatomes and Peripheral Nerves - Segmental Innervation of the Skin and the Peripheral Nerve Supply (Anterior and Posterior)#… | Peripheral nerve, Nerve, Neurology
Mapping of dermatomes of the lower extremities based on an animal model in: Journal of Neurosurgery Volume 82 Issue 6 (1995)
Mapping of dermatomes of the lower extremities based on an animal model in: Journal of Neurosurgery Volume 82 Issue 6 (1995)
Dermatomes: Anatomy and dermatome map | Kenhub
Which of the following is not a neurotransmitter? A) Acetylcholine B) Dopamine C) Dermatome D) Noradrenaline | Study.com
Mapping of dermatomes of the lower extremities based on an animal model in: Journal of Neurosurgery Volume 82 Issue 6 (1995)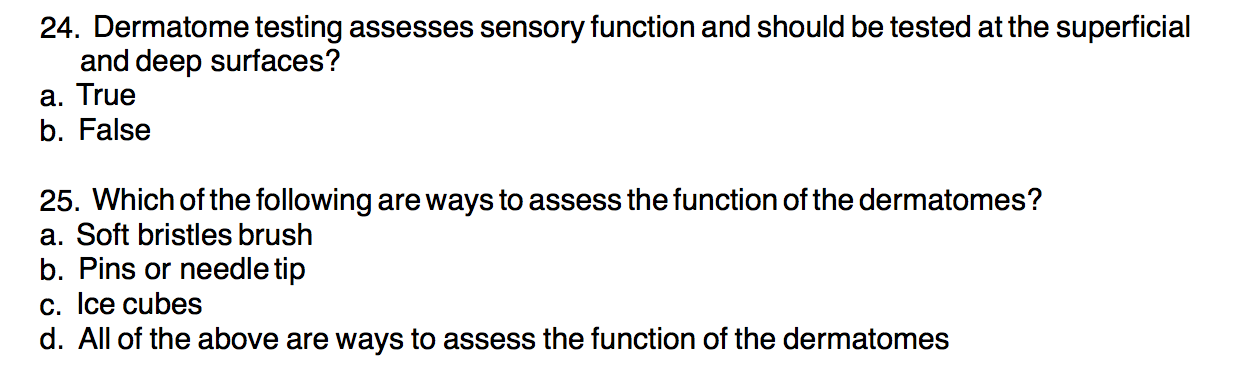
Solved: 24. Dermatome Testing Assesses Sensory Function An... | Chegg.com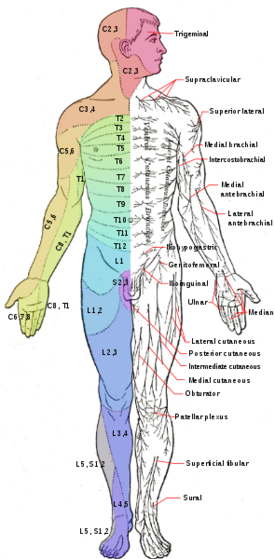
Lumbar Radiculopathy - Physiopedia
3 TRUTHS UNIVERSITY DIDN'T TELL YOU ABOUT RADICULAR SYNDROME | Physiotutors
Dermatome (anatomy) - Wikipedia
Overview of Spinal Cord Disorders - Brain, Spinal Cord, and Nerve Disorders - Merck Manuals Consumer Version
Chiropractic Adjustment
Clinical Anatomy of the Dermatomes and Innervation of the Joints | SpringerLink:background_color(FFFFFF):format(jpeg)/images/article/en/dermatomes/sBtx6ViucBogaqVxMEQozQ_xzgcUgTfrHfK3Q2dWKNTOQ_L1.png)
Dermatomes: Anatomy and dermatome map | Kenhub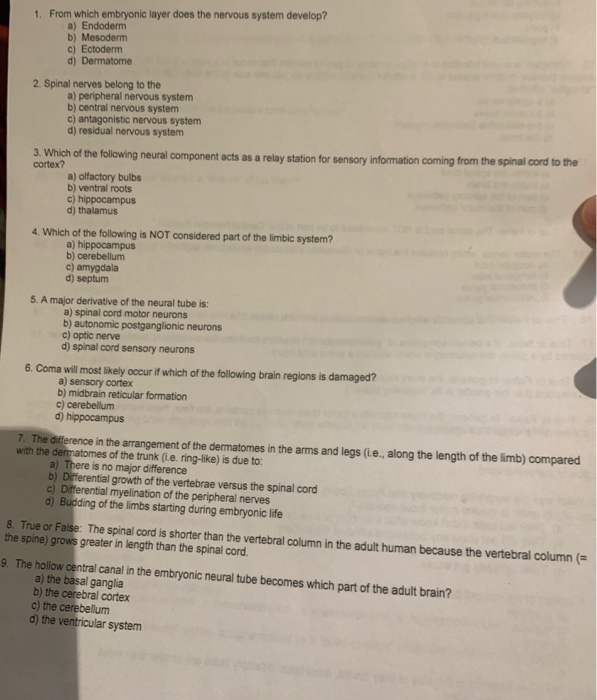
Solved: 1. From Which Embryonic Layer Does The Nervous Sys... | Chegg.com
Perceptual threshold to cutaneous electrical stimulation in patients with spinal cord injury | Spinal Cord
Description of sensation sparing from dermatomes T10-S3, L1-S3 and S3 | Download Table
 Solved: Which Of The Following Statements Is True Regardin... | Chegg.com
Solved: Which Of The Following Statements Is True Regardin... | Chegg.com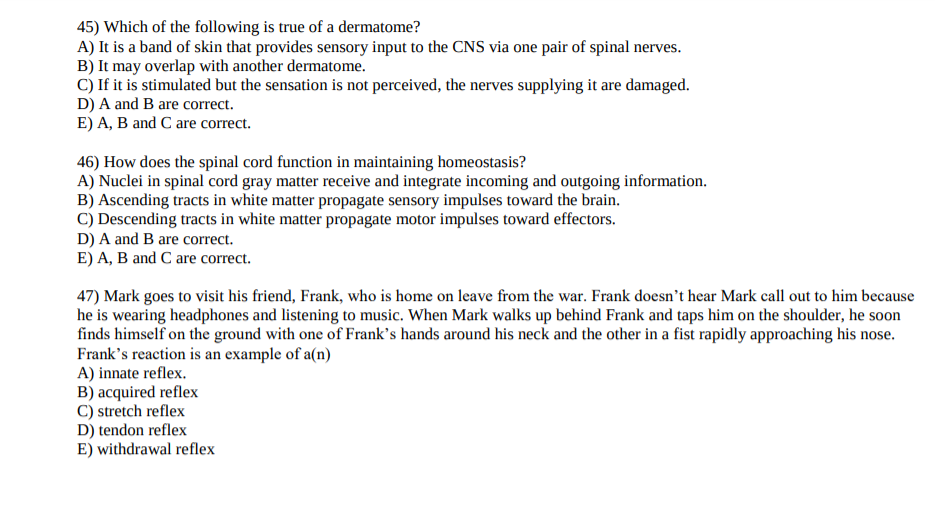























:background_color(FFFFFF):format(jpeg)/images/article/en/dermatomes/sBtx6ViucBogaqVxMEQozQ_xzgcUgTfrHfK3Q2dWKNTOQ_L1.png)


Posting Komentar untuk "which statement about dermatomes is true?"